Bedsores, or pressure sores, are injuries affecting a person’s skin and the underlying tissue. They occur when there is prolonged pressure to the skin, creating a rash which can progress to something much worse. They usually occur over a bony area such as your heels, sacrum, hips, elbows, or ankles. Bedsores occur when pressure is applied to soft tissue causing blood flow to be obstructed to that tissue. They are common in those who are not moving, such as being bedridden.
Types of Bedsores
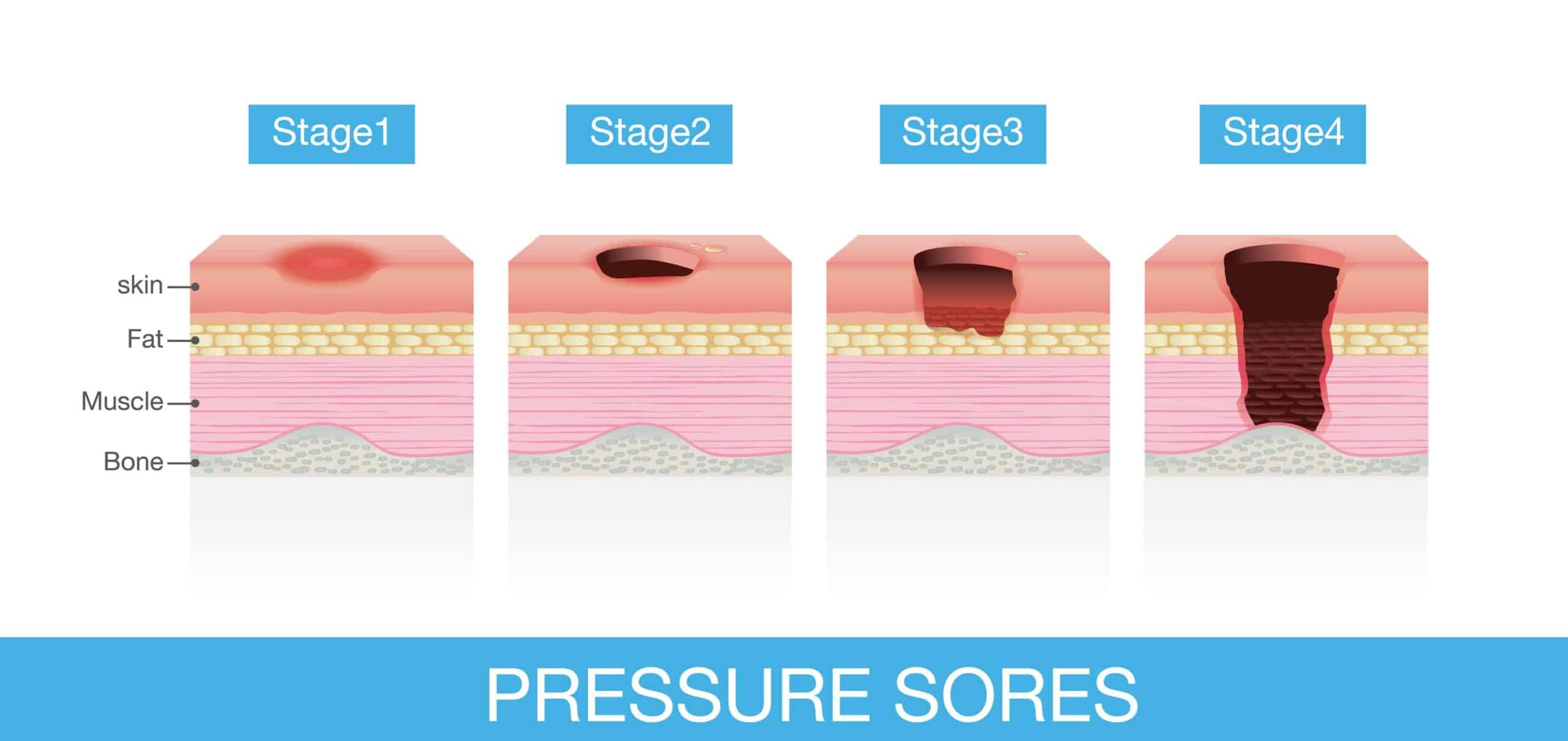
While unfortunately, bedsores can be common, especially for the elderly population, there are varying degrees of seriousness when it comes to bedsores. Specifically, there are 4 types of bedsores:
- Stage I: During this stage the bedsore is just beginning to form. The skin will not be broken, but you could see a red mark starting to appear. This mark may or may not be tender, painful, or warm.
- Stage II: At this stage the bedsore will morph into an open wound. The outer layer of skin will have been destroyed and the sore will be pink or red in color. The wound should be shallow and may look like a blister.
- Stage III: The bedsore will have changed from being shallow to deep. This means the skin loss will have been extremely serious and fat may now be showing. The skin inside the sore will be dead or a yellow color.
- Stage IV: This is the most serious type of bedsore. It can mean the loss of tissue, including muscle and tendons. With the loss of these the bone may be showing through the hole in the skin. Dead tissue, which may be yellowish or dark and crusty, may appear around the edges or even at the bottom of the open wound.
Risk and Signs
According to the U.S. National Library of Medicine, the following groups may be at risk of developing bedsores, or pressure ulcers:
- If you spend most of your day in a bed or chair;
- If you are overweight or underweight;
- If you are unable to control your bowels or bladder;
- If you have decreased feeling in an area of your body; and/or
- If you spend a lot of time in one position.
Early signs of pressure sores include:
- Skin redness
- Warm areas
- Spongy or hard skin
- Breakdown of the top layers of skin or a sore
Prevention
Bedsores are preventable, and in fact are easier to prevent than to treat. Changing positions is the key to preventing pressure sores. Remember, they are able to form because of the consistent pressure in one area; movement will allow for blood flow to occur in areas susceptible to bedsores. The changes in position need to be frequent and the particular positions of the body need to minimize pressure on those areas vulnerable to bedsores. Additionally, keep skin clean and dry. This will help to keep pressure sores from developing. Also, drink plenty of water every day—hydration helps! As stated above those bedridden, or who spend most of their time in a wheelchair, are more prone to bedsores. According to the Mayo Clinic, here are some ways to help with prevention of pressure ulcers in both of those situations:
Repositioning in a wheelchair recommendations:
- Shift your weight frequently. Shifting your weight about every 15 to 20 minutes is very helpful. Also, ask for help with repositioning about once an hour. Doing so will take pressure off certain areas and maintain blood flow.
- Lift yourself, if possible. If you have enough upper body strength, do wheelchair pushups — that is, raising your body off the seat by pushing on the arms of the chair.
- Look into a specialty wheelchair. Some wheelchairs allow you to tilt them, which can help relieve pressure.
- Select a cushion that relieves pressure. Use cushions to relieve pressure and help ensure your body is well-positioned in the chair. Various cushions are available, such as foam, gel, water filled and air filled. Make sure to sit on a foam or gel seat cushion that fits your wheelchair. Also, natural sheepskin pads are helpful in reducing pressure on the skin. DO NOT sit on donut-shaped cushions since they actually reduce blood flow.
Repositioning in a bed recommendations:
- Reposition yourself frequently. Change your body position every one to two hours.
- Look into devices to help you reposition. If you have enough upper body strength, try repositioning yourself using a device such as a bar above the bed. Additionally, caregivers can use bed linens to help lift and reposition an individual. Repositioning can help reduce friction and shearing. Never drag yourself to change your position or get in or out of bed, this can cause skin breakdown. Get help if you need moving in bed or getting in or out of bed.
- Try a specialized mattress. Use special cushions, a foam mattress pad, an air-filled mattress or a water-filled mattress to help with positioning, relieving pressure and protecting vulnerable areas. Your doctor or other care team members can recommend an appropriate mattress or cushion.
- Sheets and clothing should be dry and smooth. Make sure there are no wrinkles.
- Adjust the elevation of your bed. If your hospital bed can be elevated at the head, raise it no more than 30 degrees. This helps prevent shearing.
- Use cushions to protect bony areas. Protect bony areas with proper positioning and cushioning, you can use a soft pillow or soft foam to place between parts of the body that press against each other or the mattress. Rather than lying directly on a hip, try lying at an angle with cushions supporting the back or front. You can also use cushions to relieve pressure against and between the knees and ankles. You can cushion or lift your heels with cushions below the calves. DO NOT put pillows under your knees, as this puts pressure on your heels.
Prevention Technology
Even with all these practical tips, wouldn’t it be great if modern technology could also help out? Well, that time may have come. Leaf Healthcare, Inc. has developed a wireless system that monitors a patient’s position, movement and activity to document, and thus, help with the management of mobility protocols for those at risk due to immobility. The device, known as a Leaf Patient Sensor, electronically monitors patients’ positions and movements, recording each time a patient is moved and alerting caregivers when patients need to be repositioned. This could be extremely helpful in a hospital and nursing home setting. As technology and medical advances improve, hopefully the extremes in which people can be exposed to bedsores decreases. Unfortunately, bedsores are more common in neglectful situations. If you found this blog informative, you may also be interested in the following:


